Vessel Loop Alternative
DermaClose–A much needed update to the traditional vessel loop technique.
The technique of dermatotraction for closure of fasciotomy wounds was first described by Cohn in 1986 using vessel loops. Today, vessel loops are commonly performed by interlacing elastic vessel loops over the wound through staples placed at the skin edges.
The procedure is quick, technically simple, and utilizes readily available equipment. However, the vessel loops technique suffers from a number of drawbacks:
- The thin loops frequently do not have adequate tensile forces to allow for closure of large wounds, especially those compromised by significant soft tissue swelling
- The swelling often causes vessel loops to break
- Dressing changes are difficult, and carries with it the potential of staples becoming dislodged
- Unequal distribution of force across the wound edges is not ensured with vessel loops
- Vessel loops require constant maintenance and retightening
- There is no way to really know if the tension applied is adequate (is too strong or too weak?)
DermaClose is superior to vessel loops in multiple ways
The DermaClose Continuous External Tissue Expander is indicated for use in reducing or assisting with the closure of full-thickness wounds of the skin. DermaClose is the only controlled-force, self-tightening, continuous external tissue expander.
- Once set, DermaClose automatically maintains the proper amount of tension and does not need to be readjusted or tightened.
DermaClose gently and rapidly expands the skin on the subcutaneous planes around the wound until the edges are brought close enough together for final suturing and closure.
In addition, DermaClose gives you precise control. You know the tension set is optimal.
Several authors have also done direct comparisons of DermaClose vs vessel loops and have found that, as published by Flemming et al in the Annals of Plastic Surgery, “although effective, this technique has not proved nearly as powerful as the Dermachose device.”
| DermaClose improves | DermaClose reduces |
|---|---|
How DermaClose works
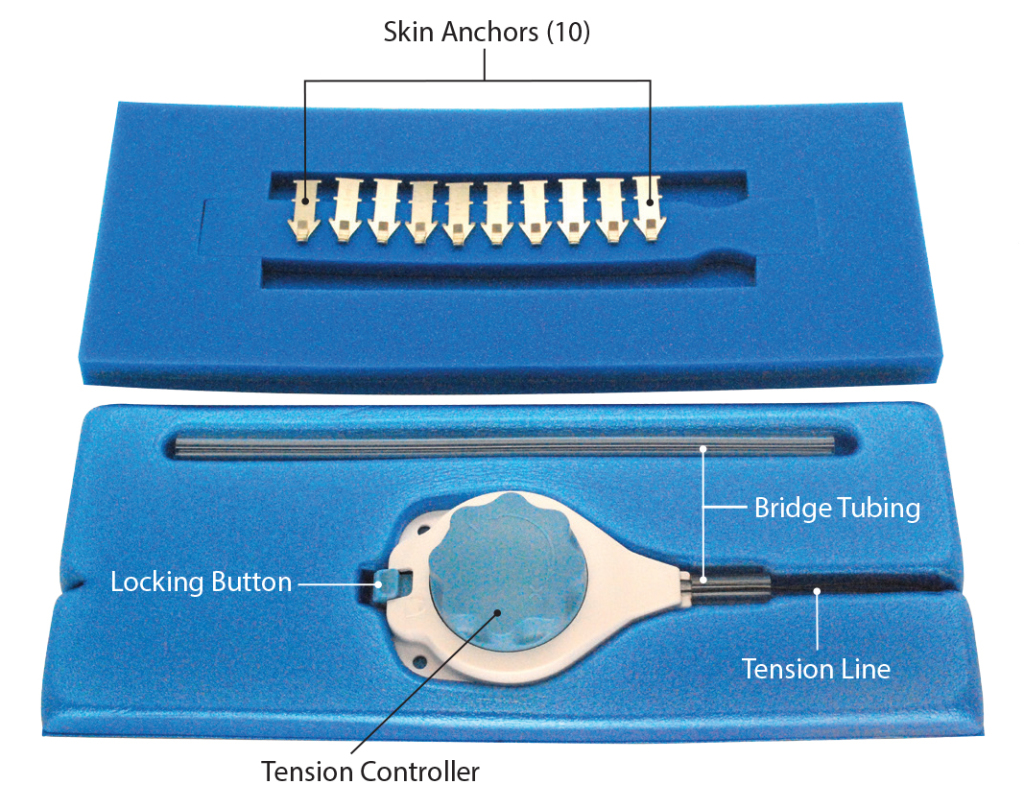
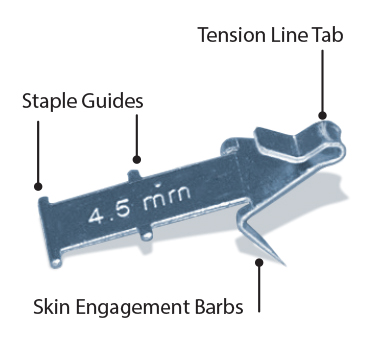
DermaClose utilizes skin anchors (made of 316L surgical stainless steel) which are inserted into the skin with the tips approximately 0.5 cm to 1 cm from the edge of the wound. These anchors penetrate 4.5 mm into the subcutaneous tissue and each anchor is then secured with a standard skin stapler.
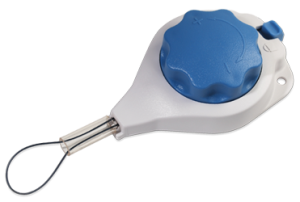
Once the anchors are in place, the line from the DermaClose tension controller is attached around each skin anchor in a shoelace configuration and the knob of the tensioning device is rotated until a clutch mechanism provides an audible indication that full tension has been achieved.
It is a sterile, single patient use device. A 3M skin stapler is included with the kit. The tension controller is just 1.7 inches wide, 2.6 inches long, 0.8 inches high and is made of ABS plastic. The nylon suture loop is 66 cm long.
Typically one DermaClose is used per each 10 cm of length of the wound. For wounds that are 10 cm or more wide it is recommended to use one DermaClose XL per 10 cm of length. Multiple devices can be used for large wounds. The new DermaClose XL device comes with a 95cm loop of line.
Give your patients a less painful, more cosmetically appealing option
In many cases, patients need not suffer through the additional pain and complications of skin grafts. DermaClose provides a viable alternative. DermaClose is indicated for use in reducing or assisting with the closure of full-thickness wounds of the skin.
DermaClose is a continuous external tissue expander that facilitates rapid tissue movement to reduce or reapproximate wounds. Once the initial application has been completed the DermaClose device does not require any additional tightening.
Proven in 15,000 cases, 20 clinical publications, and 42 case reports.
Clinical publications
Annals of Plastic Surgery
August 2014 (Vol. 73, Issue 2, pp 183-189)
Fleming ME, O’Daniel A, Bharmal H, Valerio I.
Application of the orthoplastic reconstructive ladder to preserve lower extremity amputation length.
Applying various concepts, including DermaClose, to the reconstructive ladder may allow for viable soft tissue coverage to maximize functional outcome…READ MORE
To review on the publisher’s website, click here.
 Annals of Plastic Surgery
Annals of Plastic Surgery
October 2012 (Vol. 69, Issue 4, pp 418-421)
Gabriel F. Santiago, MD,* Benjamin Bograd, MD,* Patrick L. Basile, MD,*Þþ Robert T. Howard, MD,*Þ Mark Fleming, DO,* and Ian L. Valerio, MD, MS, MBA*Þþ
Soft Tissue Injury Management With a Continuous External Tissue Expander
Overall time to wound coverage ranged from 1 to 6 days, with mean time to definitive wound coverage being 4.4 days. The mean decrease in wound surface area in this group was 74.3%…READ MORE
To review on the publisher’s website, click here.
 Archives of Facial Plastic Surgery
Archives of Facial Plastic Surgery
September 2012
Ashley G. O’Reilly, MD; William R. Schmitt, MD; Randall K. Roenigk, MD; Eric J. Moore, MD; Daniel L. Price, MD Arch Facial Plast Surg.
Published online September 03, 2012. doi:10.1001/archfacial.2012.662
Closure of Scalp and Forehead Defects Using External Tissue Expander
To describe the novel use of an external tissue expander in the reconstruction of scalp and forehead defects. A prospective review was performed on 7 patients who underwent extirpation of head and neck malignant neoplasms resulting in scalp and forehead defects. Reconstruction was performed using an external tissue expander device. Patient clinical factors, defect size, and photographs were collected. READ MORE
To review on the publisher’s website, click here.
Case studies
16 years old female
Presentation: Olecranon fracture with necrosis and split thickness skin grafting of the antecubital wound.
Size of wound: 8 x 8 cm with tethering to muscle
Time to closure: 4 days
Vac use: No
Outcome: Nearly 95% of the graft was excised. Patient is extremely happy with aesthetics and improved function.
50-year-old male
Presentation: The patient presented with atopic dermatitis and a large, poorly differentiated squamous cell carcinoma of the upper back. The carcinoma was excised resulting in a 15cm x 16cm deficit.
Injury: Atopic dermatitis and squamous cell carcinoma of the upper back
Surgeon: Dr. Robert G. Chandler, MD
Size of wound: 15cm x 16cm
Time to closure: 2 days
Vac use: No
Outcome: At follow-up 6 weeks later, the wound had healed nicely
Photos
Product literature
Download a skin graft vs DermaClose comparison, reimbursement information, ICD 10 codes, and a quick reference guide.