A proven alternative to skin grafts
DermaClose helps prevent the complications, pain, and scarring associated with skin grafts
Skin grafting is a well-established and fundamental technique that Podiatry surgeons commonly use to help close cutaneous wounds secondary to trauma, following amputations and for chronic ulcerations. However, the technique is susceptible to a variety of complications leading to graft failure. Most commonly these include:
- Hematoma or seroma
- Poor take and/or contraction (due to shearing forces)
- Infections
- Rejections
- Misplacing the graft dermis side up (a less frequent, but still common error)
- Poor cosmetic appearance (mismatched texture, color, or topography which may require additional surgical correction)
Skin grafts should only be employed when other methods of reconstruction such as primary closure, healing by secondary intention (or delayed primary healing), or local skin flaps are inappropriate, unavailable, or would produce a suboptimal result.
And because all grafting procedures require a donor site wound, which is created when the graft is harvested, that procedure itself is subject to potential risks and complications. Often, the secondary defect is the slowest to heal, and it is the source of most of the postoperative discomfort.
Common indications for STSGs
STSGs are most commonly used when cosmesis is not a primary concern or when the defect to be corrected is of a substantial size that precludes the use of an FTSG. Other uses of STSGs are the coverage of chronic unhealing cutaneous ulcers, temporary coverage to allow observation of possible tumor recurrence, surgical correction of depigmenting disorders with the use of suction blister grafts to line cavities such as the orbit, and coverage of burn areas to accelerate wound healing and to reduce fluid loss.
Common indications for FTSGs
FTSGs is indicated in defects where adjacent tissues are immobile or scarce or if the adjacent tissue has premalignant or malignant lesions which precludes the use of a flap.
Anatomical locations well suited to FTSGs include:
- Nasal tip
- Helical rim
- Forehead
- Eyelids
- Medial canthus
- Concha
- Fingers and toes
FTSG are also used when multi-staged procedures are not advisable.
Give your patients a less painful, more cosmetically appealing option
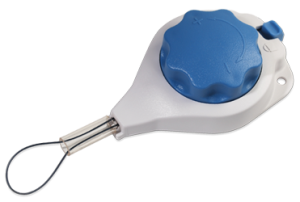
In many cases, patients need not suffer through the additional pain and complications of skin grafts. DermaClose provides a viable alternative. DermaClose is indicated for use in reducing or assisting with the closure of full-thickness wounds of the skin.
DermaClose is a continuous external tissue expander that facilitates rapid tissue movement to reduce or reapproximate wounds. Once the initial application has been completed the DermaClose device does not require any additional tightening.
Proven in 15,000 cases, 20 clinical publications, and 42 case reports.
Clinical publications
Annals of Plastic Surgery
August 2014 (Vol. 73, Issue 2, pp 183-189)
Fleming ME, O’Daniel A, Bharmal H, Valerio I.
Application of the orthoplastic reconstructive ladder to preserve lower extremity amputation length.
Applying various concepts, including DermaClose, to the reconstructive ladder may allow for viable soft tissue coverage to maximize functional outcome…READ MORE
To review on the publisher’s website, click here.
 Annals of Plastic Surgery
Annals of Plastic Surgery
October 2012 (Vol. 69, Issue 4, pp 418-421)
Gabriel F. Santiago, MD,* Benjamin Bograd, MD,* Patrick L. Basile, MD,*Þþ Robert T. Howard, MD,*Þ Mark Fleming, DO,* and Ian L. Valerio, MD, MS, MBA*Þþ
Soft Tissue Injury Management With a Continuous External Tissue Expander
Overall time to wound coverage ranged from 1 to 6 days, with mean time to definitive wound coverage being 4.4 days. The mean decrease in wound surface area in this group was 74.3%…READ MORE
To review on the publisher’s website, click here.
 Archives of Facial Plastic Surgery
Archives of Facial Plastic Surgery
September 2012
Ashley G. O’Reilly, MD; William R. Schmitt, MD; Randall K. Roenigk, MD; Eric J. Moore, MD; Daniel L. Price, MD Arch Facial Plast Surg.
Published online September 03, 2012. doi:10.1001/archfacial.2012.662
Closure of Scalp and Forehead Defects Using External Tissue Expander
To describe the novel use of an external tissue expander in the reconstruction of scalp and forehead defects. A prospective review was performed on 7 patients who underwent extirpation of head and neck malignant neoplasms resulting in scalp and forehead defects. Reconstruction was performed using an external tissue expander device. Patient clinical factors, defect size, and photographs were collected. READ MORE
To review on the publisher’s website, click here.
Case studies
16 years old female
Presentation: Olecranon fracture with necrosis and split thickness skin grafting of the antecubital wound.
Size of wound: 8 x 8 cm with tethering to muscle
Time to closure: 4 days
Vac use: No
Outcome: Nearly 95% of the graft was excised. Patient is extremely happy with aesthetics and improved function.
50-year-old male
Presentation: The patient presented with atopic dermatitis and a large, poorly differentiated squamous cell carcinoma of the upper back. The carcinoma was excised resulting in a 15cm x 16cm deficit.
Injury: Atopic dermatitis and squamous cell carcinoma of the upper back
Surgeon: Dr. Robert G. Chandler, MD
Size of wound: 15cm x 16cm
Time to closure: 2 days
Vac use: No
Outcome: At follow-up 6 weeks later, the wound had healed nicely
Photos
Product literature
Download a skin graft vs DermaClose comparison, reimbursement information, ICD 10 codes, and a quick reference guide.